To provide you with a more personalized experience, this website may place cookies on your computer. By accepting cookies you agree to this use of your data under Quantician’s Privacy Policy.
Making Sense of eCQMs: Why Electronic Clinical Quality Measures Matter in 2026

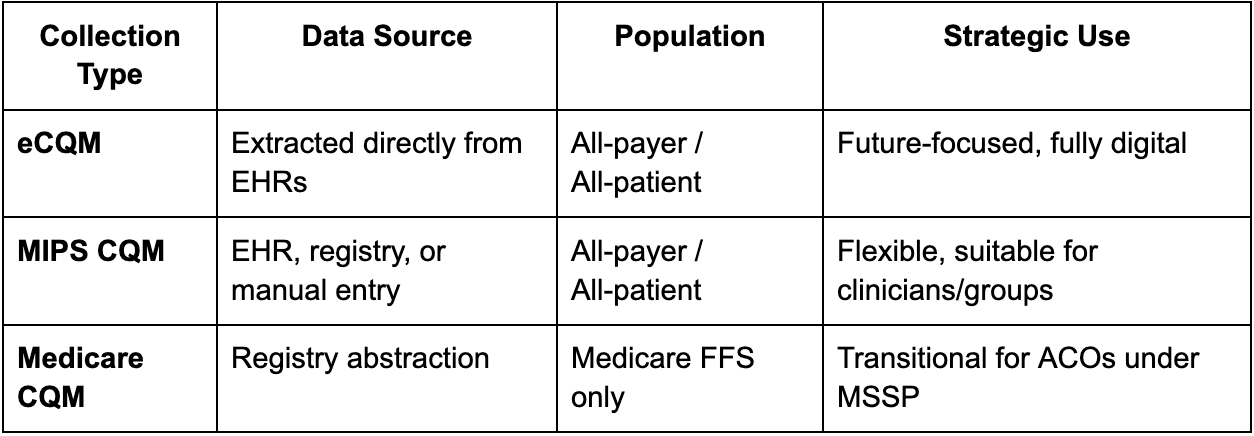
Every year healthcare shifts toward digital quality measurement and understanding how to report quality data correctly has never been more important. For 2026, three reporting types dominate CMS programs: eCQMs, MIPS CQMs, and Medicare CQMs. Each affects compliance, scoring, and strategy differently.
Below, we break down what each means, how they compare, and which path may serve you best in the 2026 performance year.
The Basics eCQMs (Electronic Clinical Quality Measures) eCQMs use structured data extracted directly from certified EHR or health IT systems to evaluate care quality. They’re fully digital and built for interoperability, using standardized formats and value sets to align care data across programs.
MIPS CQMs (Merit-based Incentive Payment System CQMs) MIPS CQMs can pull from any valid data source: EHRs, claims, or even manual chart review. They offer flexibility for clinicians and groups participating in the Quality Payment Program but are less automated than eCQMs. Often times requiring the use of additional CPT2 codes or new workflows.
Medicare CQMs Introduced for ACOs in the Shared Savings Program, Medicare CQMs mirror MIPS CQMs but focus only on the ACO eligible Medicare Fee-for-Service beneficiaries. They serve as a transitional option for organizations still building toward all-payer, all-patient digital reporting.
Key Differences at a Glance
Why eCQMs Are the Future CMS continues to move toward digital quality measurement (dQM), signaling that eCQMs are the long-term direction. The agency has already stated that the MIPS and Medicare CQM options will likely be phased out once ACOs have adopted digital measurement infrastructure.
eCQMs also support real-time performance insight, standardized data capture, and multi-payer alignment, allowing organizations to close care gaps faster and more efficiently. For many, 2026 is the right time to make the transition.
Choosing the Right Path
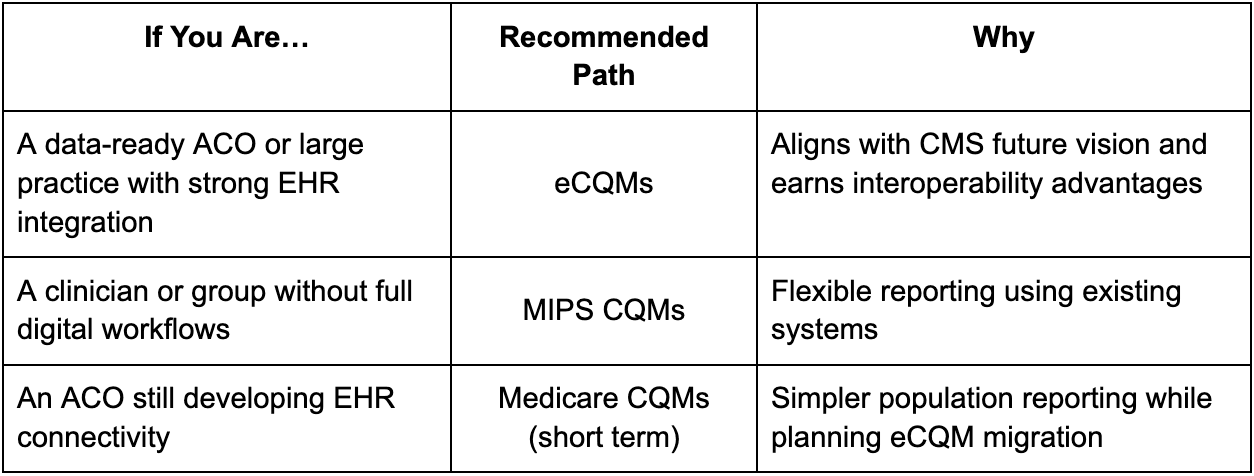
Rule of thumb: eCQMs are the most sustainable, MIPS CQMs the most flexible, and Medicare CQMs the most temporary.
Preparing for 2026
- Confirm program eligibility and measure set: MIPS, MSSP, APM, etc.
- Assess your EHR readiness: Can your data be extracted electronically?
- Ensure complete population coverage: Medicare FFS or All-payer
- Engage a CMS-qualified registry: Registries like Quantician collect, validate, and securely submit your data accurately
- Plan for eCQMs now: Even if you use MIPS CQMs or Medicare CQMs in 2026, the goal is digital alignment by 2027 or 2028.
The Bottom Line For ACOs and clinicians preparing for 2026 reporting, eCQMs represent an opportunity for clarity, automation, and readiness for the next phase of value-based care.
Partnering with a CMS-Qualified Registry like Quantician ensures data integrity, interoperability, and peace of mind across every submission path whether a team is ready for full digital reporting or building toward it.

ACO Quality Reporting: What’s Required & How to Do It Right

What ACO Leaders Need to Know About the Proposed MSSP Changes

