To provide you with a more personalized experience, this website may place cookies on your computer. By accepting cookies you agree to this use of your data under Quantician’s Privacy Policy.
Automate Chart Audits with AI Coding Reviews
Quantician enables users to quickly pinpoint suspected coding inconsistencies through AI powered technology. We help assure that all relevant conditions are identified and supported by documentation within the patient’s chart.
Learn more
Learn more about our quality coding solutions
Contact Sales
Contact our sales department today

Quantician confirms all relevant codes are identified using AI technology to autonomously review charts and claims.
Quantician uses AI to identify applicable HCC codes that have been included on a previous claim but not resubmitted in the past 12 months. The tool also has the ability to review unstructured text in each patient chart to identify HCC codes that have been recorded in the documentation but never added to a claim.
Leveraging modern technology, our solutions enable users to significantly increase efficiency and accuracy of medical billing in value based reimbursement models. By calculating the risk score for each patient, Quantician allows a care team to focus their efforts on patients with the highest risk or most complex medical needs. Clinicians can then tailor a personalized treatment plan that uniquely addresses the patients specific condition.
Coding accuracy
Patient Risk Scoring
Create data driven treatment plans that are personalized to each patient’s unique needs.
Risk adjustment
Predict costs
Care gap identification
Claims processing

Providing customized solutions
Clinical Documentation
Our team of experts help overcome unique challenges with the people, processes and technology we deploy.
Charting accuracy
Workflow design/automation
Data validation audits
Analytics and Reporting

Keep Learning
Read best-practice articles about performance, development and more.

January 12, 2026
Making the Deadline: A Path to PY 2025 Submission
CMS has opened PY 2025 QPP submissions. Learn key deadlines, how to submit MIPS data, and what to review before the March 31, 2026 cutoff.
1 min read

December 15, 2025
The 2025 MIPS Hardship Exception Application
Learn how the 2025 MIPS Hardship and EUC Exceptions work, who qualifies, key deadlines, and how to avoid penalties during reporting disruptions.
2 min read
November 19, 2025
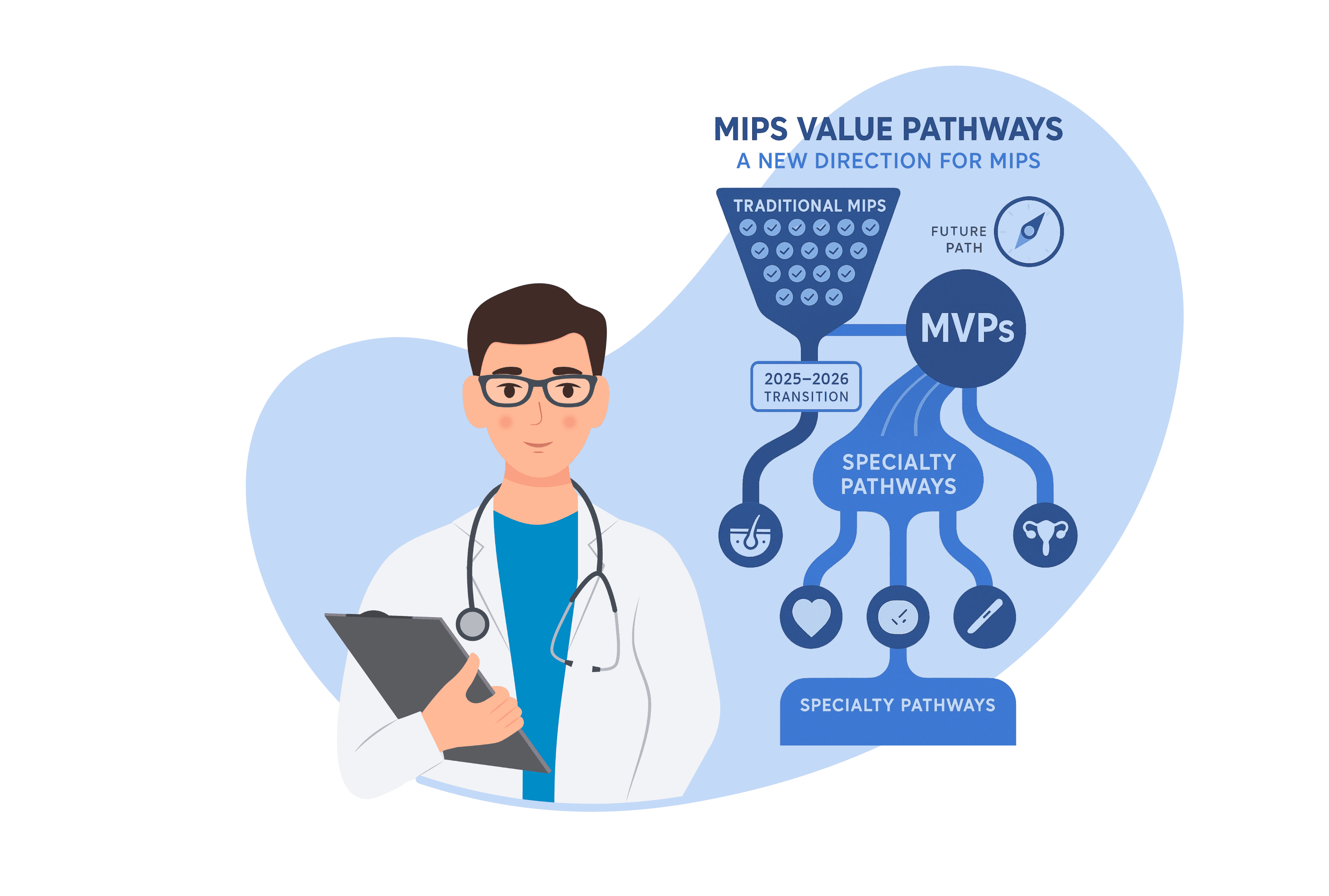
MIPS Value Pathways (MVPs): A New Direction for MIPS
Explore how MIPS Value Pathways (MVPs) are reshaping CMS reporting, offering specialty-specific, digital-ready quality reporting for clinicians and ACOs.
4 min read
How Does Quantician Work?
Quantician integrates with nearly all EHR, PM and Payer data sources which enables it to present users with valuable insights. This data can be used to close care gaps, automate workflows and make strategic decisions.
Solutions
Support
Contact