To provide you with a more personalized experience, this website may place cookies on your computer. By accepting cookies you agree to this use of your data under Quantician’s Privacy Policy.
MIPS Value Pathways (MVPs): A New Direction for MIPS
The way clinicians report quality and performance to Centers for Medicare & Medicaid Services (CMS) is changing and fast. By 2026, MVPs will become the next major step toward specialty-specific, digital-ready performance reporting. MVPs aim to simplify reporting for clinicians and bring more meaningful, specialty-aligned insight to quality data.
For accountable care organizations (ACOs), this shift signifies a new opportunity to support participating providers. MVPs aid in aligning performance metrics, reducing admin burden, and helping them succeed under a new framework.
What Are MVPs? MVPs are a redesigned reporting option under the Merit‑Based Incentive Payment System (MIPS), created by CMS to align reporting with specialty, condition, or patient-population frameworks, rather than a broad “one-size fits all” measure set.
Specifically, MVPs consist of:
- A focused set of quality measures, including one outcome or high-priority measure.
- Improvement activities and cost measures aligned to that specialty/condition.
- A foundational layer common to all MVPs: the Promoting Interoperability (PI) category + population health measures based on claims data.
For the 2025 performance year, CMS finalized 21 MVPs available for reporting, covering specialties from women’s health to dermatology to surgical care.
MVP participation remains voluntary for 2025, though CMS has signaled that traditional MIPS may be phased out in the future.
Why Participate in an MVP?
- Reporting That Fits The Practice: Instead of picking measures from a long list, MVPs align to specialties or conditions. This means reporting reflects real-world work, such as cardiology, urology, or primary care.
- Reduced Burden, Increased Relevance: With a narrower, more relevant measure set, providers can avoid chasing metrics that don’t reflect their patient mix. For 2025, MVP participants need only one improvement activity (instead of multiple) and no separate population health measure selection.
- Strategic Readiness for the Future: CMS has clearly indicated that MVPs are the “future path” for MIPS reporting. Starting early allows for a head-start on workflows, data capture, and strategic alignment.
- How ACOs Can Add Value: For an ACO supporting multiple participating providers, MVPs offer a way to standardize reporting across specialties, streamline data collection, and strengthen provider engagement. With MVP selection support, aligning EHR/registry workflows, and monitoring performance, an ACO can enhance overall network quality scores and reduce the administrative burden on individual practices.
How Reporting Differs with MVPs (vs. Traditional MIPS)
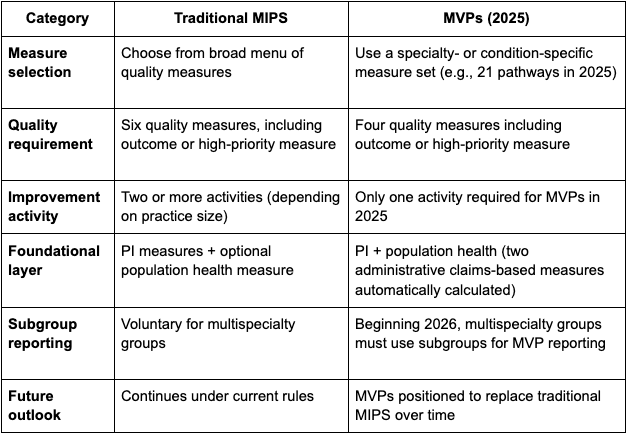
The Scoring Methodology After the MVP data submission period concludes, providers should expect to receive MVP Performance Feedback. Much like with traditional MIPS, this includes 3 phases of feedback and comparative feedback on performance - highlighting how performance compares at the category level to other participant scores on the same MVP. The performance phases are as follows: preliminary feedback, final scoring and comparative feedback, and a payment adjustment phase (during which participants have 30 days to submit a targeted review).
*Note: MVP categories and associated score weights remain unchanged from Traditional MIPS.
The Intentions Behind MVPs CMS developed MIPS Value Pathways to begin making the shift towards aligning measures to specialty and clinical workflows, rather than generic reporting. Next is to reduce the burden on providers and make reporting more meaningful, while guiding providers and organizations to the new era of the MIPS framework - value-based care, integrated cost, quality, interoperability, and population health.
How to Prepare for 2026 Understanding the intentions behind CMS’s new direction is one step, knowing how to apply and prepare that understanding in another. To prepare for MVP reporting, begin with the following: 1. Identify Your Pathway: Review the finalized MVPs for 2025 and select the one(s) that best match the specialty or condition (for example “Value in Primary Care” or “Dermatological Care”). 2. Plan for Subgroup Reporting (if applicable): If part of a multispecialty group, begin planning for subgroup formation, as subgroup reporting becomes required in 2026 for MVPs. 3. Align Data & Workflow: Ensure the EHR or registry can capture the required data elements, support the specialty-specific measures, and handle the foundational layer (PI + population health). 4. Test & Benchmark: Conduct internal reviews, run performance dashboards, identify data gaps and begin testing submission workflows now to avoid an unprepared approach. 5. Choose the Right Partner: Work with a CMS-qualified registry or vendor experienced in MVP reporting. They can help with registration, measure tracking, data submission, and performance feedback.
Meeting Deadlines and Reminders Being prepared for MVPs means recognizing deadlines and nuances to avoid surprises and stay adaptive. Here are upcoming deadlines to be aware of and a look into the administrative claims measures that can either maximize your score or place it in jeopardy.
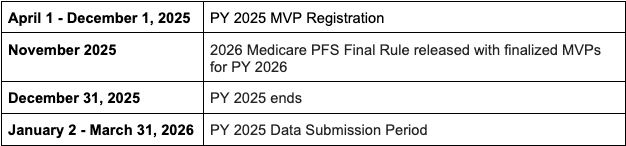
*Administrative Claims Measures: For the 2025 MVPs, CMS will automatically calculate the cost and population health measures through administrative claims-based data associated with lives attributed to them under each measure. This means specific claims-based measures are not selected by the MVP participant.
Final Thoughts MVPs aren’t just an option to select, they are shaping the next era of MIPS reporting. For clinicians and groups, they bring greater relevance, less burden, and stronger alignment to care delivery. For ACOs, they offer a platform to support and unify participating providers around meaningful, specialty-based metrics.
Getting ahead of the MVP transition in 2025 and 2026 means being positioned to lead. Excel in MVP reporting today and beyond by learning more about MVP readiness here.

CY 2026 Medicare PFS Final Rule: A Strategic Overview for Registries, ACOs & Reporting Partners

Digital Quality Measures

